A few weeks into the new medication, she complained of stomach pain a few times. We dismissed it. A few days later, she had a painful episode at school and they called us to pick her up; her school aide mentioned it seemed like constipation. We attempted to treat for that with fluids and juice. Another episode of pain here and there, both at home and school, and we tried other remedies. One day, it seemed so bad that we gave her a suppository to encourage movement. Every time, she seemed fine after a while.
When the neurology appointment finally came, Chris pushed that we needed her off the medication if seizures were not likely to recur, since it was causing constipation. The doctor thought that was strange; constipation is not a common side effect of Keppra. They want her to stay on it, so they prescribed liquid instead to see if that helped ease her discomfort.
A few days later, she started again. It was Monday evening, and we were trying to get everyone into bed. She sat on the couch and just screamed. We tried drinks of water, heating pad, rubbing her belly, snacks to distract her, but nothing calmed her down. She can’t really communicate specifics, but she can clearly say, “MY TUMMY HURTS!” and then she screams. After an hour, we were both exasperated and gave in; if we couldn’t help, we had to take her to the hospital.
We hated this idea; it was late, we have been so, so busy and didn’t need an all night constipation monitoring trip. She seemed in pain, and we figured she needed an ultrasound or x-ray to rule out anything more serious. I dressed her, Chris packed a bag and then took off with her into the night.
They waited in the ER all night. She was given some pain medication and quieted down, but still was uncomfortable. I tried to sleep while the kids slept, worrying about what a mess I would be the next day at work. I woke at 5, and started to strategize with Chris, who had not slept at all.
They still hadn’t had an ultrasound, but they were waiting for one. If he couldn’t leave the hospital by 6, there was no way for him to get home in time for me to get to work in time. The kids needed to get to school, too. Another crazy night, another round of emergency sub plans; I would head in after lunch for a half-day.
I got Benny and Evie to school and picked up around the house while I waited for news. The ultrasound finally analyzed, they had an inkling of a problem - she had gallstones, and they could not rule out her appendix. Appendix I could understand, but gallstones?! Straight out of left field.
The details began to come together. Gallstones, and gallbladder was badly infected, causing pain. She needed it removed. She was being admitted for surgery. Because of her shunt, she needed IV antibiotics to prevent the infection in her abdomen from spreading to the tubing that leads to her brain. Her current shunt has lasted a notable many years and any infection could lead to needing it replaced.
We felt terrible. We had been dismissing her pain for days and weeks. We had been treating her for constipation, which was one issue, but was likely not the root cause of her pain. We had been impatient and irritated with her complaints, overwhelmed by her being sent home from school and frustrated with her inability to stay calm about what we thought was minor discomfort. She historically responds very dramatically to minor issues, so we just thought she was putting on a show for attention…poor girl. I still feel terrible. It’s one of the issues we deal with regularly, her being unable to clearly communicate what she thinks, feels, needs or wants. We try to interpret what is happening, take her words, drawings, actions and routines into account to figure it out, and sometimes we miss the mark. Usually it is something minor; this was serious.
I met Chris at the hospital after working for a few hours. He hadn’t slept for over 40 hours and was exhausted. I got there just in time to move Scarlett from the ER to the surgical floor; she would have surgery sometime the following morning. I got reacquainted with the inpatient procedures and spaces - she hadn’t been admitted in many years. She got a “dinner” tray of clear fluids and I settled in for a night of semi-restful sleep on the same fold-out chairs that I had spent weeks in almost 13 years ago.
Surgery happened first thing the next morning. She was prepped and ready by 8:00. We woke early when the morning nurse was doing vitals. As soon as she saw me awake, the nurse introduced herself, gave me a quick rundown of the plan, and then told me she remembered us. She had been one of the nurses who cared for Scarlett in the days before she went into surgery, in January 2011, the last time we were on that floor. She remembered Scarlett, and me, very vividly, and was so happy to see how well she was doing (other than the gallbladder part!)
We got down to the surgical waiting room, and the doctor came out to ask her which bandaids she wanted - she chose princesses. We gave her a pre-anesthesia sedative - she gets very anxious with any kind of procedure now, so medicating her before putting on a mask or starting a procedure that will scare her is calmer and safer. Once she was asleep, I walked to the cafeteria for some coffee.
Surgery took about 2 hours. I met her back in the recovery room. A nurse came in while we were waiting, and asked if this was Scarlett. She said, “She’s been here before, right?” I said yes, but it has been quite a while. She responded, “I remember. She had two EVDs (external ventricular drains - “brain drains”) in the window space of the PICU.” I was shocked - that was exactly right, almost 13 years ago. I confirmed that this was in fact her, and we joked that it must have been quite an experience for her to remember after all this time.
She had 4 small incisions on her belly that seemed to cause her very little discomfort. The surgeon explained that there was a lot of adhesions throughout her abdomen from her shunt, so it had been rather challenging to reach her gallbladder, so despite the small holes, a lot had happened inside. He was not as reassuring about solving her pain; he hoped that this would help, but pain is hard to track and he couldn’t guarantee this would be the end.
I asked what in her history might have led to this; surely something so strange was caused by some medication, procedure or illness in her complex medical history….but no. They insisted that is was most likely unrelated, just a fluke. Gallbladder issues are becoming more common, especially among females. I am not fully convinced that this is the end of that, but I haven’t had a chance to dig further.
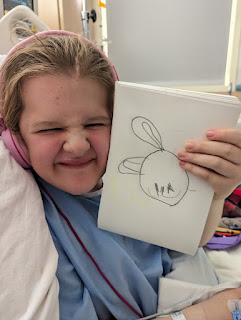
The rest of the hospital stay was uneventful. Two days of IV antibiotics and pain management, which Scarlett spent primarily in bed watching her tablet and coloring. She loved having her meals delivered on demand and getting to wear a hospital gown that matched the walls and curtains.
She came home on Friday. Within 5 minutes of getting in, she ran to the trampoline and started jumping. She was in no pain and we gave no pain medication after discharge, not even Motrin. She went back to school the following Monday and has been pain free so far. She might have some digestive issues related to her lack of gallbladder as time goes on, but should otherwise be okay.





No comments:
Post a Comment